Exasperating Israel’s patients – A health system that has lost its way by Dan Ben-David The
horrifying murder of a nurse at a clinic last month is an extreme case among
hundreds of assaults on Israeli health care workers every year. As in the case of reckless drivers who kill
others, the guilty ones are those who inflict the harm. Period. Since
the human spectrum encompasses not only the normative, but also the careless
and the crazy, is placing a cop in every clinic and street intersection the
solution? Shouldn’t these fringes be
accounted for more fully in the planning stages? Rather than being content with charging
drivers who run over others who stop on road shoulders, wouldn’t it be
preferable to widen the shoulders and move back the guardrails so that drivers
won’t have to change a flat tire while their bodies protrude onto the road? Where
have the hospital beds gone? It
is similar with healthcare. When Israel
was young, it not only built towns and roads but also research universities and
hospitals. The number of curative
(acute) care hospital beds managed to keep pace with Israel’s phenomenal
population growth from 1948 until the late 1970s, when the country’s priorities
changed. Since then, for decades on end,
the number of hospital beds per capita in Israel has been falling steadily. Today, Israel is situated today beneath nearly
all of the OECD countries (see figure). 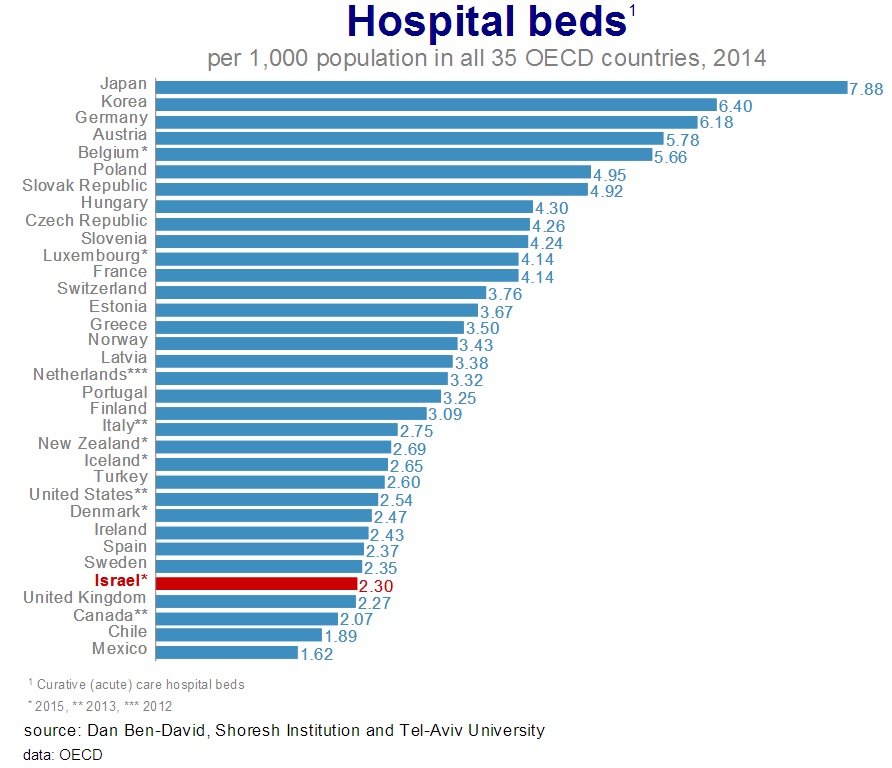
This
may be a positive outcome in the eyes of policy-makers who feel that it is
wanton to waste precious resources on empty hospital beds. But it is tantamount to claiming that roads
need to be utilized by the maximum number of vehicles possible. This may indeed be the prevailing line of
thinking in Israel’s governments since congestion on the country’s roads (as
measured by the number of vehicles per kilometer road) has swelled to three
times the OECD average. This has
happened even though Israel has 38% fewer vehicles per capita than the OECD
average. If
this is the Israeli approach for gauging efficiency, maybe the time has come to
find alternate measures. There is no
doubt that fewer beds per person imply greater utilization of very expensive
healthcare assets. But avoiding
overflows during peak seasons requires accommodating slack during other
periods. A
relatively young population doesn’t need many beds since young people fall ill
less frequently, and Israel’s population is younger than most in the developed
world. However, today the country’s
population older – and the country is wealthier – than it was three decades
ago. Despite this, Israel funded 60%
more beds per capita in 1988 than it does today. So the problem is not just vis-à-vis
other countries. The situation has
deteriorated compared to Israel itself many years ago. Hospitals
with the highest occupancy rates in the developed world It’s
possible to claim that in modern countries, there are alternatives that are
preferable to hospitalization.
Maybe. But if there were such
alternatives in Israel, we wouldn’t be witnessing the appalling – and frequent
– sights of patients lying in hospital corridors and dining areas, deprived of
any privacy at their most vulnerable hour. Israel’s
insufficient investment in hospital beds has yielded an occupancy rate of 94%,
greater than in any other OECD country and a quarter higher than the average (75%)
of all the other countries in the organization (see figure). This is an annual average for an entire
country that does not reflect the tremendous pressures that develop during peak
seasons in some of the most populated areas.
Efficient? Possibly. But the result is considerable misery in
shameful hospitalization conditions for the patients and their families. All too often the result is friction and
violence – not to mention reduced hygiene at hospitals, with all this
implies. As if this were not enough,
Israeli patients face an additional challenge, severely undermanned medical
staffs. 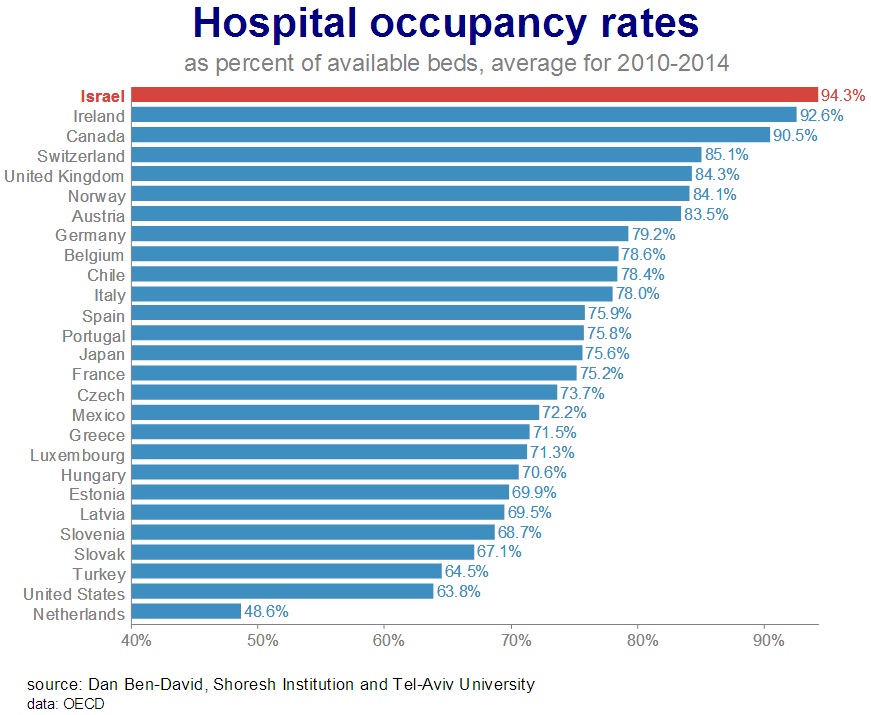
Steady decline in
the number of nurses – toward the bottom of the developed world The
number of active nurses per capita in
Israel is extremely low compared with the OECD average. Since the beginning of the 2000s, the average
number of nurses per capita in the OECD has risen by a third. In Israel, this number has declined by about
a tenth. Consequently, the number of
nurses per capita in Israel was three-quarters of the OECD average in 2000,
falling to about half the OECD average just over a decade later (see figure). 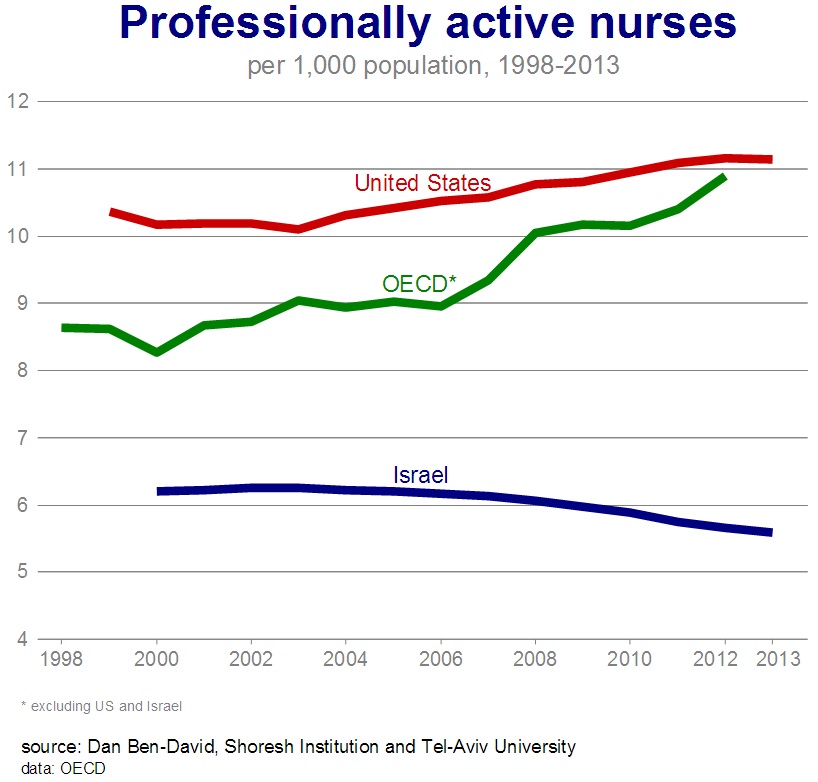
Even
more troubling is the picture of nurse flows – the annual number of nursing
graduates – because it underscores the direction Israel is headed. The average number of nursing graduates in
the OECD (47 per 100,000 population) is nearly three times the Israeli number
(16), which is near the bottom of the group (see figure). 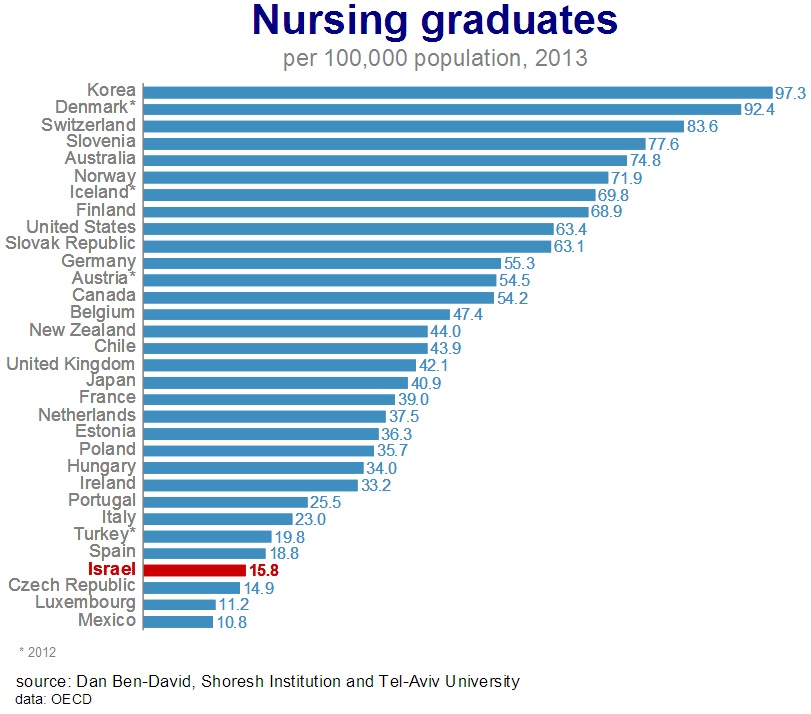
How
can the country’s sick and weak be expected to cope when they most need care
and attention? Is it any wonder that
some of the less stable among them go nuts?
Are cops the solution, or maybe it’s time to consider a significant
change in Israel’s national priorities?
Not only can such overcrowding with such a small nursing staff drive
people crazy, it’s also dangerous. Number
1 in infectious diseases Hospitalization
conditions in Israel are like a huge petri dish – breweries for infections and
diseases. The share of Israelis dying
from infectious and parasitic diseases is the highest in the OECD. When taking into account the number of deaths
from such diseases by different age groups and standardizing the populations of
the various developed countries to enable a more accurate comparison, it’s
clear that Israel is in a league of its own.
The number of deaths from infectious and parasitic diseases (35 per
100,000 population) is 50% (!) greater in Israel than in the second place
country, Mexico (23 per 100,000 population), and almost twice the OECD average
excluding Israel (see figure). 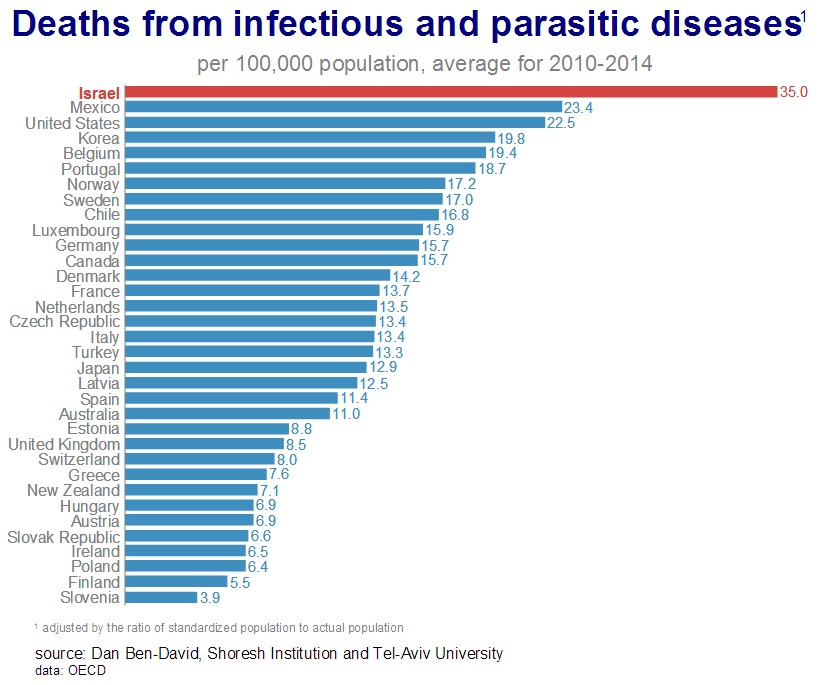
Of
course, not all deaths from infectious and parasitic diseases are related to
hospital conditions. Yet the number in
Israel is extraordinary. Anyone who
thinks that Israel and the developed world are at least converging should think
again. There has been a vast gap between
Israel and the OECD average since the 1970s (see figure).
While the number of deaths per capita from infections in the OECD has
been stable, even falling slightly, it has been on a deafening takeoff in
Israel over the past two decades. Since
implementing healthcare reform in 1995, the number of deaths per capita from
infectious and parasitic diseases in Israel has doubled. 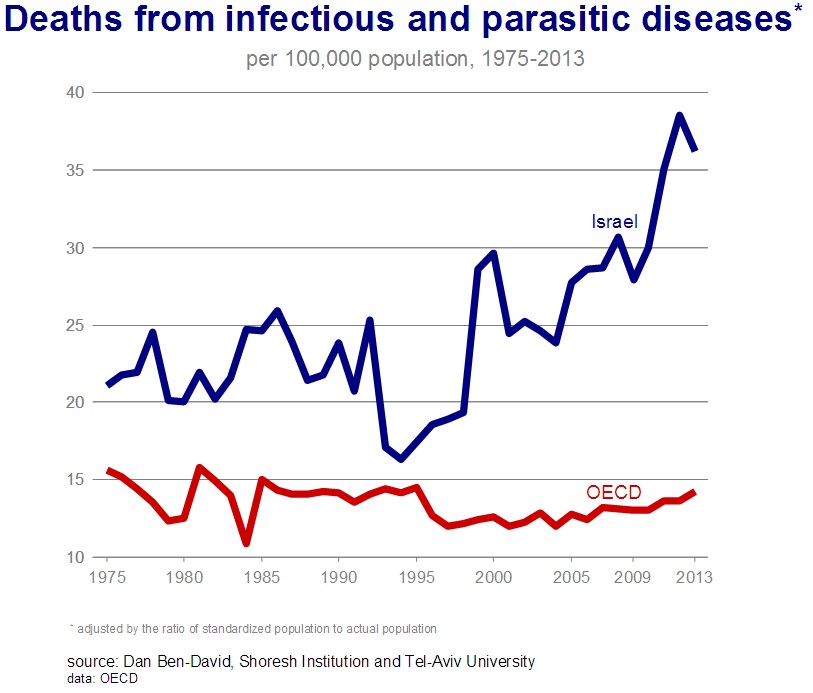
It’s
possible to gain a perspective on the problem’s severity when comparing it to
other issues that receive widespread public attention: The number of people
murdered in terror incidents reaches double digits each year while the number
of traffic fatalities reaches the hundreds.
But the number of Israelis dying from infectious diseases is in the
thousands every year. This isn’t
destiny. It’s in our hands. Money isn’t
lacking. The problem is the way money is
used, and who’s paying. Clearly,
overcrowding, a paucity of nurses and the great number of deaths from
infectious diseases don’t represent the overall picture of Israel’s health
system. Often, the country’s high
life-expectancy rates coupled with its low healthcare expenditures are
presented as an indication of the system’s efficiency. Life-expectancy in Israel is definitely one
of the highest in the world, due in part to doctors and nurses trained at the
highest international professional standards.
Mediterranean diets and other idiosyncratic factors also contribute to
longevity in Israel. At
first glance, Israel’s national healthcare expenditure (as a percent of GDP, to
enable international comparisons) appears to be relatively low. In fact, it’s lower
than the national healthcare expenditure of 71% of OECD countries. However,
a major reason for the low expenditure has less to do with the system’s
efficiency and more to do with Israel’s fairly young population. The older a population, the higher the
mortality rates and healthcare spending.
When national healthcare expenditures are normalized by the relative
weights of the various age groups and their mortality rates, the expenditure
picture in Israel’s case of Israel flips.
It turns out that Israel’s normalized healthcare expenditure is higher
than that in 76% of the OECD countries.
So we’re a bit less efficient than it appears. National
healthcare e xpenditures may be divided into public and private
expenditures. Public healthcare
expenditures (after normalizing for population age groups) as a share of GDP
put Israel in the middle of the OECD ranking.
On the one hand, it is not particularly high or low compared with the
rest of the developed world. But
Israel’s population is aging at one of the fastest rates in the developed
world, and it takes years to train the personnel and build the necessary infrastructures
to deal with this phenomenon. The
source of Israel’s high national expenditures are its private
expenditures. While private healthcare
expenditures in Israel (after normalizing and dividing by GDP) aren’t even
close to American private expenditures, they’re still higher than the private
expenditures in three-quarters of the developed countries (see figure). 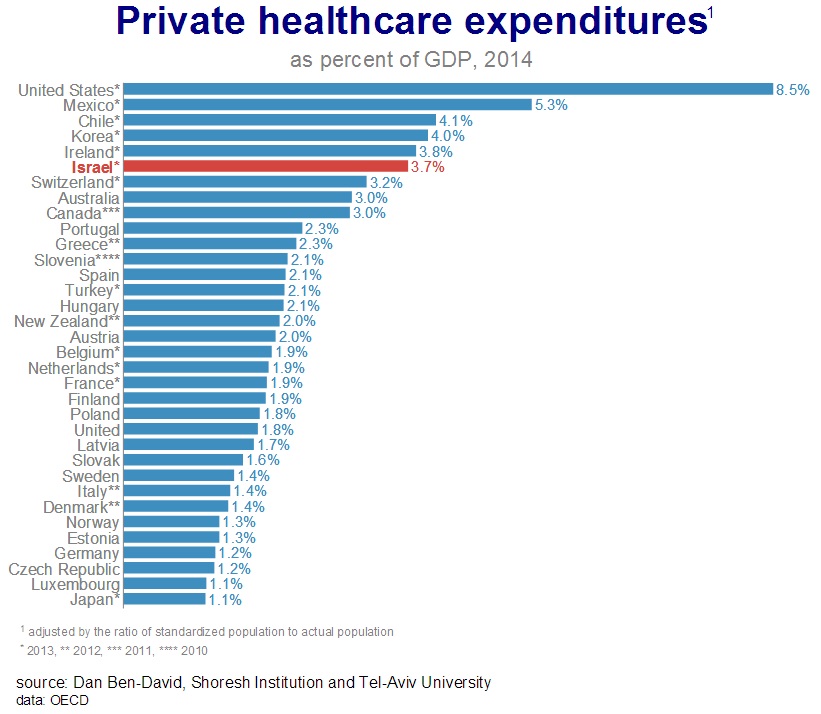
Israel,
with income and education gaps among the highest in the developed world, needs
to ask itself if it also seeks similar distinctions in healthcare
provision. This is the implication when
the share of private expenditures is high.
Not everyone can bear this burden.
Furthermore,
exasperating patients isn’t an essential ingredient in extending
life-expectancy. Family and friends
cannot replace hospital nurses. Corridors
need to be for passage and dining areas for eating. Patients should be hospitalized only in
hospital rooms – and they shouldn’t be infected by those around them. There is no greater pain than the loss of
loved ones to unnecessary infections. The
question of questions: what kind of health system does Israel want? Health
systems encompass one of the most complicated problems in economics. These are systems in which two of the three
key sides determine what the third side will pay. In the United States, patients and physicians
decide how much insurance companies pay.
In Israel, it’s the insurance companies/health maintenance organizations
and physicians who decide what patients pay – whether in terms of money, waiting
periods or health. Therefore,
the healthcare question in Israel is considerably greater than the issues
raised here. How is it possible to
compensate quality healthcare professionals at rates that will attract them to
the profession, and retain them, while maintaining an adequate expenditure
level for an Israeli society, half of whose members don’t even reach the bottom
rung of the income tax ladder?
Considering that just 20% of Israelis already account for 90% of the
country’s entire income tax revenue, the answer doesn’t lie in increasing the
burden even further on those narrow shoulders, but rather in a significant
change in Israel’s national priorities. The
time has come for a different allocation of the limited national budget in
directions that benefit the greater good rather than narrow and sectoral
interests. But it’s not enough to throw
money at a problem and hope that it resolves itself. Instead of endlessly looking for symptomatic
patchwork solutions that create inherent inconsistencies, the time has come to
provide an answer to the big question – what kind of a health system does
Israel want in another decade? Only then
will it be possible to build it from the existing pieces and add the necessary
missing parts. The
socio-economic discourse in Israel is problematic on three main tiers of
discord. First, basic concepts are not
understood by many of the debaters. For
example, when comparing incomes over time, inflation needs to be
discounted. This is done by reporting
incomes in terms of constant prices which are specified for a particular
year. This is the source of the mistake
made by those who claim that the rise in incomes among the lower income deciles
between 1990 and 2006 did not surpass the price increases. The
second tier of the problematic discourse regards the blinders resolutely worn
by many of those presenting facts to an unsuspecting public. One side of this debate extols the virtues of
economic growth without mentioning that, in its current form, many individuals
are barely able to cope. The more market
failures there are – and in Israel, there are many – the greater the number of people
finding it difficult to make ends meet, and consequently, the greater the
economic gaps. The
opposing side in this debate issues reports and statements that do not contain
a trace of corroboration for President Kennedy’s adage, “a rising tide lifts
all boats.” This, despite the fact that
from 1967 through 2006, economic growth in Israel contributed to an increase –
in constant prices – of 275% in the poor’s living standards, as indicated by
the rise in average gross incomes in the bottom decile of families. However, since the wealthy benefited much
more from the growth, this turned into the only aspect of the growth process
publicly put forth by this side of the debate. On
the third tier of the problematic public discourse are the plethora of superficial
and radical headline-grabbing proclamations.
These prevent a broad internalization of the big picture – one that is
substantially worse than what is brought to the fore by the usual spokespersons
from the various sides. For over two and
a half decades, behind the scenes and outside the radar screens of the
politicians and advocacy research centers, gross income inequality soared
upwards along a trajectory as straight as a ruler. This steady increase, of 20% in the Gini
index between 1979 and 2006, transformed Israel into one of the least equal
countries in the Western world. It is
important to note that gross income inequality reflects the actual level of
income disparity, the level that would exist had it not been for the existence
of the social safety net of taxes and welfare. A
country that does nothing to prevent this actual increase in inequality must
then implement rear-guard tax and welfare policies in order to reduce net
income gaps. This is what Israel did. During the years 1979-2000, net income
inequality – which is what the public debate focuses on – rose by “only” 4%. As
a result, welfare payments had to rise steadily and steeply – not to reduce
inequality, but to prevent the continuously-rising gross income gaps from being
reflected in net income gaps. In 1980,
defense spending was roughly similar to the combined expenditures on education,
health and welfare. Since then, the
former has fallen and the latter have risen.
Today, the amount that Israel spends just on welfare is greater than its
entire defense expenditure. It is a
trajectory that will have an unhappy ending if not stopped in time. This decade, we received a glimpse of what
the future holds. The defense situation
and the recession prevented continued increases in welfare spending, and this
led to a substantial increase in net income inequality. Despite
the relentless barrage of strident public statements that would have us believe
otherwise, the twin objectives of heightened growth and lower income inequality
do not conflict with one another.
Treating the root sources of these problems requires – but is not
limited to – comprehensive structural reforms in the realms of education and
employment to increase the number of people who will be able to help themselves
and to contribute to their country. But
the State of Israel – its elected officials and unelected advocacy research
centers – continue to focus on cosmetic and artificial solutions as substitutes
for the real thing. When
the dependent segment of the population is growing larger by the day, it is
important to understand that there exists a point of no return. Laws that are difficult to pass today in the
Knesset will be impossible to pass in another generation. |